 Inflammatory Cytokines and PTSD – Review of evidence and cytokine storm in COVID-19
Inflammatory Cytokines and PTSD – Review of evidence and cytokine storm in COVID-19
SE theory has important implications for how to develop person-centered interventions that address the biopsychosocial impacts of post-acute COVID-19.
In the 2018 article on, ‘Dysregulation of inflammation, neurobiology, and cognitive function in PTSD’ the authors explore the impact of the body's inflammatory system in Post-Traumatic Stress Syndrome (PTSD). These have wide-ranging implications for trauma treatment and addressing the impacts of post-acute COVID-19.
SE theory indicates that the dysregulation from exposure to traumatic events would impact multiple health systems and that increased regulation in the autonomic nervous stem allows dysregulated systems to return to more healthy functioning. It is well documented that individuals with PTSD have elevated inflammatory cytokines, a key biological system in immune function, tissue health, and neurobiological functioning.
Impacts of dysregulation in immune functioning along with impacts to cognitive functioning and emotional processing are common with increased levels of inflammatory cytokines. Addressing inflammation through medication management and biopsychosocial interventions, such as re-establishing autonomic regulation, has significant promise for improving health.
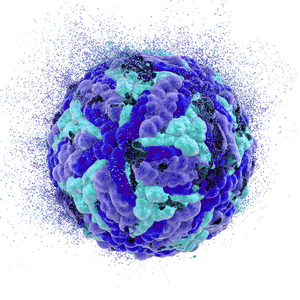
One of the clearest pathways that COVID-19 leads to long-term COVID symptoms and even death is called ‘cytokine storm.’ Cytokine storm is a fundamental dysregulation in the cytokine system where elevated inflammation leads to tissue damage, and tissue damage leads to increasing inflammation, turning into a positive feedback loop of increasing inflammation and tissue damage.
Individuals with Post-COVID Syndrome (PCS) have significant disruptions in inflammation processes that can lead to risk for multiple systemic challenges such as headaches, cognitive processing challenges, mental health symptoms, and multiple health challenges. It is possible that a combination of restoration of autonomic regulation, trauma-informed social support from family and community, and medical management of inflammatory processes could improve clinical outcomes for people with these deeply life-impacting processes.
SE research and protocols into interventions, if developed and tested, could be an important support for reducing the risk of PCS and improving the quality of life for those with PCS.
Read More: https://link.springer.com/article/10.3758/s13415-020-00782-9
Quinones, M. M., Gallegos, A. M., Lin, F. V., & Heffner, K. (2020). Dysregulation of inflammation, neurobiology, and cognitive function in PTSD: an integrative review. Cognitive, Affective, & Behavioral Neuroscience, 20(3), 455-480.

